Did you know that people who struggle with drinking or substance use disorder who engage in long-term, consistent care have a 75% chance of achieving sustained recovery from addiction?
It’s true. And the statistic is important because alcohol is an addictive substance and substance use is the rule, not the exception, in America.
If you’re struggling with moderating your drinking, worrying about how much you drink or are struggling with achieving sobriety, you are not alone.
Recovery from addiction is not only possible, but likely.
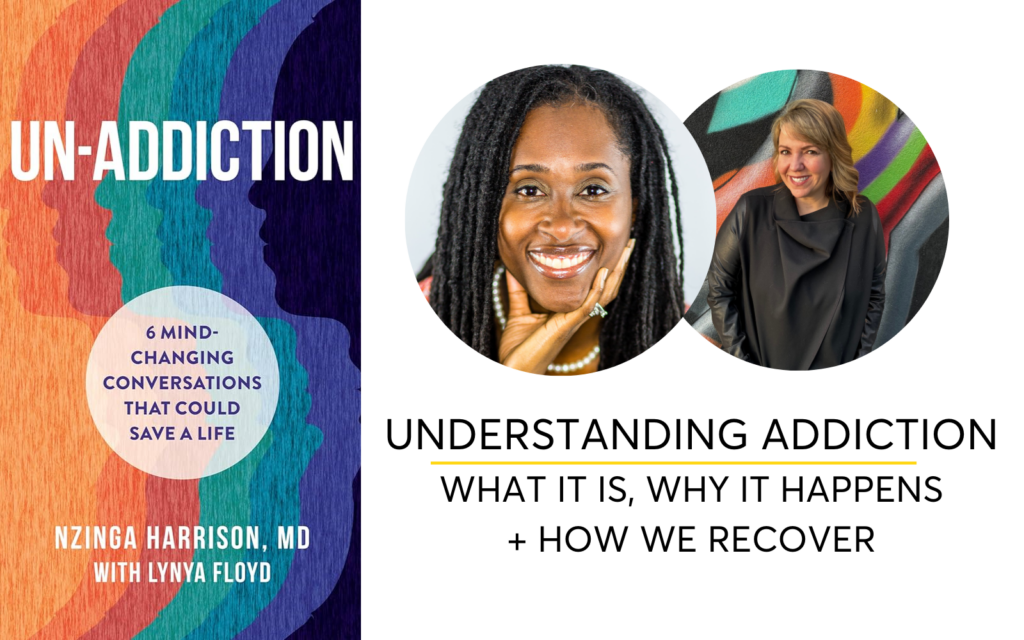
I asked Dr. Nzinga Harrison, a double-board certified physician in addiction medicine and psychiatry and the author of the book, Un-Addiction: 6 Mind-Changing Conversations That Could Save a Life, to share why addiction is often misunderstood as a moral failing rather than a medical condition. Through our conversation you’ll have a new understanding of what addiction is, why addiction happens and how we can recover from addiction to alcohol or other substances.
It’s Time to Change the Way We Talk About Addiction, Relapse and Recovery.
So is “relapse is part of the illness” of addiction? The short answer is no.
You may have heard that two-thirds of people who experience a relapse in the first few months of recovery, but that’s only a small part of the story.
I tried for years to drink less and take breaks from alcohol because I was worried that I was drinking too much. I would get 4 days and drink, 7 days and drink, 2 weeks and drink. I felt like it was impossible to reach even 30 days alcohol-free.
But when I added on-going, consistent support to navigate my first few weeks, 6 months and year sober I achieved long-term, sustained recovery. After drinking a bottle of wine a night for decades I have not had a drink in over 8 years.
Getting out of the drinking cycle is hard. It’s normal to struggle to stop drinking if you’re physically experiencing cravings for alcohol, if you don’t have tools to navigate drinking events, communicate your needs or decision to stop drinking and if you don’t have support.
But remember, 75% of people with substance use disorder who engage in long-term, consistent care achieve sustained recovery from addiction.
So, what’s the most important part of that sentence?
In order to recover from substance use disorder you need to engage in long-term, consistent care. You deserve ongoing support and treatment, much like the management required for other chronic illnesses.
You need to address the factors that contribute to drinking again and how to prevent them.
If you don’t currently have support and you’re stuck in the drinking cycle, you deserve to take better care of yourself. You don’t need to do this alone.
What would you do if you had high blood pressure, asthma or diabetes?
You would probably go to your doctor to get help and treatment to manage the chronic condition. It might take more than 30 days, or 6 weeks or 2 months to manage your blood pressure, asthma or diabetes, but you would keep working with your doctor until you got the condition under control.
The one-year relapse rates for conditions like high blood pressure and asthma are the same as—or even higher than—the relapse rates for addiction.
That’s incredible!
We need to treat addiction like any other chronic condition that can be managed with ongoing care that addresses the roots and causes of addiction to achieve long-term sustained recovery.
Long-term, consistent care for substance use disorder does not necessarily mean that you need to seek out inpatient treatment, outpatient treatment or joining and attending a 12-Step Recovery program unless that is your chosen pathway.
Dr. Harrison’s approach to addiction treatment goes beyond simply stopping substance use. She advocates for addressing the underlying factors that made addiction attractive in the first place.
This holistic approach includes managing anxiety, improving social connections, and creating a supportive environment that promotes overall well-being. The goal is not just to abstain from substances but to heal the underlying issues that drive substance use.
Here’s the support I chose to get out of the drinking cycle and happily live alcohol-free for the last 8 years.
😍 I joined an online Facebook group of people wanting to live alcohol-free
😍 I hired a sober coach to support me, listened to sober coaching audio messages, emailed her every day and had coaching sessions with her
😍 I joined a morning workout group and a running club
😍 I told my husband, my coworkers and friends that I was doing a 100 day alcohol-free challenge and then extended that challenge to 6 months and one-year alcohol-free
😍 I joined an 8 week online sober coaching program
😍 I made sober friends and started texting with them, talking to them and getting together for brunch, coffee and dinners
😍 I moved through cravings and social gatherings where I would normally drink alcohol-free and became more comfortable with that choice
😍 I started seeing a therapist weekly to work through my anxiety and create better boundaries and coping tools that didn’t include drinking
😍 I started medication to treat my anxiety and mood disorder
In her book, Un-Addiction: 6 Mind-Changing Conversations That Could Save a Life, Dr. Harrison shares that the key to successful recovery isn’t just about stopping substance use. It’s about healing the underlying issues that drive the addiction—whether that’s anxiety, social isolation, or other mental health challenges. Her approach is holistic, focusing on overall well-being, not just abstinence.
In this episode, you’ll learn:
✅ How to increase your chances of being in the 75% of people who achieve long-term sustained recovery from drinking.
✅ Why relapse is not inevitable but rather a risk that can be managed and minimized with the right support and treatment.
✅ How to change the way we talk about and treat addiction to create a more supportive and successful environment for recovery.
✅ The biological, psychological, and environmental influences that impact your risk of addiction.
✅ Why addiction should be treated like other chronic conditions, such as high blood pressure and asthma and that the one-year relapse rates for high blood pressure and asthma are the same as—or even higher than—the relapse rates for addiction.
✅ The most harmful myths about addiction that are keeping you stuck.
✅ How social and cultural environments, along with adverse childhood experiences (ACES), contribute to your addiction risk.
✅ Why Dr. Harrison hates the words addict and alcoholic.
🎉 If you’re curious about how to recover from substance use disorder, this episode is a must-listen.
Dr. Harrison will leave you informed, empowered, and hopeful about the journey to recovery.
Other resources mentioned related to Understanding Addiction
Ep. 133 with Dr. Nzinga Harrison: Know The Risk Factors of AUD
Un-Addiction: 6 Mind-Changing Conversations That Could Save a Life
In Recovery Podcast with Dr. Nzinga Harrison | Lemonada Media
Addiction medicine expert Dr. Nzinga Harrison shows us an alternative to addiction: Un-addiction
Un-Addiction Podcast with Nzinga Harrison, MD
4 Ways I Can Support You In Drinking Less + Living More
❤️ Join The Sobriety Starter Kit® Program, the only sober coaching course designed specifically for busy women.
🧰 Grab the Free 30-Day Guide To Quitting Drinking, Tips For Your First Month Alcohol-Free.
📝 Save your seat in my FREE MASTERCLASS, 5 Secrets To Successfully Take a Break From Drinking
💥 Connect with me on Instagram.
Or you can find me on Facebook, Pinterest, YouTube and TikTok @hellosomedaysober.
Love The Podcast and Want To Say Thanks?
☕ Buy me a coffee!
In the true spirit of Seattle, coffee is my love language.
So if you want to support the hours that go into creating this show each week, click this link to buy me a coffee and I’ll run to the nearest Starbucks + lift a Venti Almond Milk Latte and toast to you!
https://www.buymeacoffee.com/hellosomeday
💕 Support the sponsors of The Hello Someday Podcast
You can find all the special discounts mentioned on the show right here: https://hellosomedaycoaching.com/sponsors/
Leave me a rating and review on Apple Podcasts!⭐⭐⭐⭐⭐
I read every single review and they really help the podcast algorithm decide to share my show with a wider audience.
I’ll be forever grateful to hear from you and to read reviews like this one from Laura,
“I’ve listened to so many sober podcasts and The Hello Someday Podcast is by far THE BEST Sobriety Podcast out there for women. This podcast was key to me quitting alcohol. Casey’s practical tips and tricks are invaluable, with advice I haven’t heard anywhere else. If I could give this podcast 27 stars I would!!”
Connect with Nzinga Harrison
She is the Chief Medical Officer and Co-Founder of Eleanor Health, an innovative mental health and addiction treatment company, and have more than 20 years of experience practicing medicine. She is a double-board certified physician in addiction medicine and psychiatry with a B.S. from Howard University, an M.D. from the University of Pennsylvania, and residency training at Emory University.
She holds adjunct faculty appointments at the Morehouse School of Medicine Department of Psychiatry, serves on the Practice Management and Regulatory Affairs committee for ASAM and recently authored my first book, Un-Addiction: 6 Mind-Changing Conversations That Could Save a Life. She has also appeared in the award- winning documentary Tipping the Pain Scale, which addresses the crisis of addiction in America.
Connect with Casey McGuire Davidson
To find out more about Casey and her coaching programs, head over to www.hellosomedaycoaching.com
Want to read the full transcript of this podcast episode? Scroll down on this page.
ABOUT THE HELLO SOMEDAY PODCAST FOR SOBER CURIOUS WOMEN
Are you looking for the best sobriety podcast for women? The Hello Someday Podcast was created specifically for sober curious women and gray area drinkers ready to stop drinking, drink less and change their relationship with alcohol.
Host Casey McGuire Davidson, a certified life and sobriety coach and creator of The 30-Day Guide to Quitting Drinking and The Sobriety Starter Kit® Sober Coaching Course, brings together her experience of quitting drinking while navigating work and motherhood, along with the voices of experts in personal development, self-care, addiction and recovery and self-improvement.
Whether you know you want to stop drinking and live an alcohol-free life, are sober curious, or are in recovery this is the best sobriety podcast for you.
A Top 100 Mental Health Podcast, ranked in the top 0.5% of podcasts globally with over 1.5 million downloads, The Hello Someday Podcast is the best sobriety podcast for women.
In each episode, Casey will share the tried and true secrets of how to drink less and live more.
Learn how to let go of alcohol as a coping mechanism, how to shift your mindset about sobriety and change your drinking habits, how to create healthy routines to cope with anxiety, people pleasing and perfectionism, the importance of self-care in early sobriety, and why you don’t need to be an alcoholic to live an alcohol-free life.
Be sure to grab the Free 30-Day Guide To Quitting Drinking right here.
Subscribe & Review in iTunes
Are you subscribed to my podcast? If you’re not, I want to encourage you to do that today. I don’t want you to miss an episode.
I’m adding a bunch of bonus episodes to the mix and if you’re not subscribed there’s a good chance you’ll miss out on those. Click here to subscribe in iTunes!
Now if you’re feeling extra loving, I would be really grateful if you left me a review over on iTunes, too. Those reviews help other people find my podcast and they’re also fun for me to go in and read. Just click here to review, select “Ratings and Reviews” and “Write a Review” and let me know what your favorite part of the podcast is. Thank you!
SUPPORT OUR SPONSORS
Thank you for supporting this show by supporting my sponsors!
Learn more: https://hellosomedaycoaching.com/sponsors/
READ THE TRANSCRIPT OF THIS PODCAST INTERVIEW
Understanding Addiction – What It Is, Why It Happens And How To Recover with Nzinga Harrison
SUMMARY KEYWORDS
drinking, addiction, recover, recovery, drugs, substances, Addiction Psychiatrist, Un-Addiction, unlearn, undo things, support, 6 Mind Changing Conversations, save a life, connection, treatment, alcohol use disorder, Hello Someday podcast, sober curious, sober curious movement, alcohol-free, coping mechanism, nonalcoholic, factors, relapse, community, sobriety
SPEAKERS: Casey McGuire Davidson + Nzinga Harrison
00:02
Welcome to the Hello Someday Podcast, the podcast for busy women who are ready to drink less and live more. I’m Casey McGuire Davidson, ex-red wine girl turned life coach helping women create lives they love without alcohol. But it wasn’t that long ago that I was anxious, overwhelmed, and drinking a bottle of wine and night to unwind. I thought that wine was the glue, holding my life together, helping me cope with my kids, my stressful job and my busy life. I didn’t realize that my love affair with drinking was making me more anxious and less able to manage my responsibilities.
In this podcast, my goal is to teach you the tried and true secrets of creating and living a life you don’t want to escape from.
Each week, I’ll bring you tools, lessons and conversations to help you drink less and live more. I’ll teach you how to navigate our drinking obsessed culture without a buzz, how to sit with your emotions when you’re lonely or angry, frustrated or overwhelmed, how to self soothe without a drink, and how to turn the decision to stop drinking from your worst case scenario to the best decision of your life.
I am so glad you’re here. Now let’s get started.
Hi there.
Today, we are talking to Nzinga Harrison all about Un-Addiction.
Understanding addiction, what it is, why it happens, and how people recover.
Nzinga is the Chief Medical Officer and Co-Founder of Eleanor Health. It’s an innovative medical health and addiction treatment company, and she has more than 20 years of experience practicing medicine. Nzinga is a double board certified Physician in Addiction, Medicine and Psychiatry. Her background includes a B.S. from Howard University, an M.D. from the University of Pennsylvania and Residency training at Emory University. I also previously talked to Nzinga in Episode 133. It was an amazing conversation about what you need to know about the risk factors for alcohol use disorder. And we’re going to take that conversation further today, and so much more.
If you’re listening to this podcast, I know you love podcasts, so Nzinga also has a podcast called Un-Addiction that I will ask her all about. But in the meantime, welcome. I’m so glad you’re here again.
Dr. Nzinga Harrison 2:36
Thank you so much, and I can’t believe that was Episode 133. Like, how many since then? Right?
Casey McGuire Davidson 2:43
Oh my God, I am around 200 and, you know, by the it’ll be around 233 by the time it goes live. So incredible. I know it’s been crazy. It’s been over 4 years now. Wow.
Dr. Nzinga Harrison 2:56
I love it so much. That’s so cool.
Casey McGuire Davidson 2:59
Yeah, I do too. It’s like my favorite part of the job, well. So, I love this book. I was telling you, I’ve been reading through it, and I’ve got all the notes on it. And just to start, tell me about why you wrote this book.
Dr. Nzinga Harrison 3:13
Yeah. So, you mentioned that I’ve been practicing medicine for 20 years, and I have always been an Addiction Psychiatrist.
My passion is people who are drinking or using other drugs or substances in a way that they’re questioning. Is this how I want to be using this? Or do I think this is helping me the way it used to type of thing and really kind of like being a supportive, empowering doc to help people define what they want out of their lives, and, you know, Mark out a pathway for how to get there.
And so, I had a previous podcast. Thank you for mentioning Un-Addiction, which is the current podcast. It was called, In Recovery with Dr Harrison, and Jen Keane was a listener. And she reached out through my website and was like, I’m sure you already have a book agent, but if not, can we chat? And I was like, Oh, why would you be sure I have a book agent? Because I’m never, ever, ever, ever going to write a book. And then it’s clear who won that who won that argument? Right? 2 years later, Jen was like, You’re obviously passionate about people with addiction or people who wonder if they have it or don’t, you know, we don’t have to use the word addiction, just like one a different way. And she was like, this, will get your message out. And that’s all she had to say. And the rest is history.
Casey McGuire Davidson 4:33
Oh, that’s fantastic. So, getting the message out, that’s something that I’m really passionate about, too, and I love talking to people like you who are experts about it so much to go through in this book. But one of the first things that I think will surprise people listening to this podcast, but everyone else as well as you, talk about the 75% success rate in the context of the impact of. Long term treatment options for addiction. Can you tell me about that?
Dr. Nzinga Harrison 5:04
Yeah, so I’ll start with the name of the book. It’s a word that we made up on addiction. And kind of, how we came up with it was like, Okay, what are the things we need to unlearn that we think we know about addiction? That is like, actually, 1, wrong. 2, not helpful, too.
What are the stigma that we need to undo? That’s like, keeping people from getting support or keeping people from getting better?
And then, 3. What are the conversations we need to uncover? And that’s like the tagline for the book 6: Mind Changing Conversations that could save a life. And so, the first thing we have to unlearn is that people don’t recover.
Yeah, right, 75% of people who have struggled with a substance in whatever way consider themselves recovered or in recovery. That is 3 out of 4.
Yeah, that is more than one out of four. And one out of four is very important because, you know, one out of four is still too high. And if we can unlearn other things that we need to unlearn and undo stigma and talk about it, we could get that one to four even lower. But the medical literature tells us, for any condition that we’re dealing with, when you believe there’s a chance for you to recover, there is a better chance for you to recover. And so, we can’t only talk about devastation and people who are dying and the people that that don’t recover. We have to talk about them, but we cannot only talk about them. Can we start from a place of hope and possibility? Yeah, then figure out how we get there for more people.
Casey McGuire Davidson 6:51
I love that so much because a couple thoughts I had when you were talking about this, I remember being back in my office in my corporate job, and one of my friends who, by the way, loved wine as much as I did, you know, whatever it was, was like, hungover on Monday after some Bunco game with her girlfriends, was talking to me about the fact I don’t drink. And it, it kind of cracked me up. She was like, Yeah, but you decided to stop you didn’t have problem with alcohol. Actually, I think she put it in the present tense. She was like, you don’t have a problem with alcohol. And that cracked me up in a few ways. One, because why was it so important to her to make sure I was in X category Yeah, versus Y category? And B, what I said to her, I was like, Well, yes, I chose to stop. But alcohol is addictive, and, you know, it is designed to take you down the path of becoming more dependent on it. But B, in my mind.
I’m 8 and a half years sober now. I was like, 4 years sober at the time. I was like, I haven’t had a drink in 4 years. I have zero problem with alcohol. And Craig Ferguson at one point said, like, I can get one really quick, right? But what I loved about that is, in my mind, of like, you were hungover on Monday, I haven’t had a thing to drink in X number of years. Like, it cracks me up that you’re like, oh, but you don’t have a pro like, as if, if I had, it would be a lifelong thing. Anyway, I just, I thought that was interesting, because now I haven’t had a drink in eight and a half years, and I don’t consider myself to be struggling with alcohol at all. I just don’t touch that. That’s right.
Dr. Nzinga Harrison 8:40
No, you know, I think it’s this human phenomenon of needing to protect ourselves from the scary. So, you are colleagues working in the same job, coming in on Monday morning, kind of with a life that is similar in that way. And so, it’s probably very scary for her to see you as a person who had a problem with alcohol, because maybe that means I could also have a problem with alcohol, and this is getting to, like, undoing the stigma.
Yeah, I think the concept that we have of people that, quote, have a problem with alcohol, is homeless, drinking out of a paper bag, has lost everything, is begging for money on the street. And if you think about the whole spectrum of what, quote, “a problem with alcohol” means, it goes all the way from when I have a glass of wine, I wake up with a migraine, but I keep having a glass of wine, all the way to that very severe that I just described, but we’ve made it so scary and so dangerous to say out loud. Like, I don’t think alcohol is doing for me what I wanted to be doing. So, I’m going to stop. Like, can we just make that easy? Yeah, I don’t drink alcohol. That’s awesome. What’s next? Yeah, but it’s like, you don’t drink alcohol.
Casey McGuire Davidson 10:13
Yes, there must be summer, and I, like, back in the day when I was fully immersed in, like, wine culture and very, you know, all of my friends drank and everything else. I seriously believed that the only people who didn’t drink were, like, pregnant.
Yeah, had an issue with addiction, aka, like, they can’t drink, or were super bored, and now it cracked me up, because, like, I know so many people who don’t drink, who are incredible, but it is interesting to me.
The other thing I loved that you wrote, and I wanted to ask you about is…
So, we have this 75% success rate in terms of the context of long term treatment for addiction and recovery. And I want to dive into, like all the, every single word and piece it apart, but those are people who have sought treatment and help and support for addiction. Now there are so many people in this world, including women who contact me every day and they’re already on the path to getting support and resources, but who really struggle with this every day and don’t seek support, probably because they see it as this futile. I’ll never stop anyway. What’s point? My life will be over. It won’t work, but also it is positioned as this life sentence of deprivation and isolation and, you know, otherness from everyone they know. So, I wish that more people who struggled with addiction, drinking, whatever it is, would seek treatment because of 75% recover. That’s pretty fucking awesome, right? It doesn’t have to feel that way anymore.
Dr. Nzinga Harrison 12:09
So true. So true.
And this, these are the conversations that we have on the Un-Addiction podcast, like, what was the scariest thing for you about thinking about stopping or changing, right? Because I think that’s also important, is that the definition of recovery is not abstinence for everyone. For some people, the definition is for abstinence. For other people, the definition is different, but like, what was, what was the scariest thing? And what I hear over and over is like, I had no idea how I was going to have fun if I stopped using x. I had no idea how it was going to socialize at work, when that happens at happy hour in a bar. I had no idea how it was going to go on a girls trip with my friends and not drink, right? Like it is those things that are very, very, very important to us and culturally, at least here in the U.S. Definitely.
Other countries as well. We see alcohol as a connector, yeah, and other drugs also act as a connector for people. And so, yes, I wish it was safer for me, more people to even say. I’m not even sure this is a problem, but I think it might be.
Yeah, early intervention. Early, right? And you don’t necessarily have to, like, sign up for the life sentence of committing to never drink another drop ever again. You might get to the point where you’re like, you know what? I don’t need to drink another drop ever again. But like, let’s just start with making it safe for people to wonder, like, be curious. I wonder, if I made a change, would I feel differently in xx way that I want to feel differently and then just try it. Just try it. And that doesn’t have to be treatment for everybody.
Sometimes, I mean, I talk about connection more than I talk about treatment, and so, I think about this the same way I think about diabetes. The doctor tells you, like, oh, you know, diabetes runs in your family. Your blood sugar’s a little higher than I want it to be, even though you don’t have diabetes yet. Maybe go join the gym. The gym is not treatment, but it’s a source of connection and changing a choice that can help prevent an illness from developing, right?
Ah, you know alcohol use disorder runs in your family, and I know you’re only drinking two glasses of wine a night, but you’re telling me your mood feels a little crunchy. Why don’t we just try a month with no alcohol and see if your mood feels less crunchy? I wish we could just get to investing in people’s curiosity. Yeah, and just trying different things that doesn’t equal you have to go see Dr Harrison. She’s an addiction specialist, and she’s going to make you vow to never do X, ever again.
Casey McGuire Davidson 15:00
In your life, would you like diagnose yourself with something, or to get diagnosed, you don’t have to get diagnosed. You don’t need a label.
Dr. Nzinga Harrison 15:04
Yeah, all you need to know is you’re like, I wonder, if you wonder, we have an opportunity. Yeah,
Casey McGuire Davidson 15:15
I love that, and that’s the reason that this podcast, it’s called, you know, the Hello Someday podcast for sober curious women. Because I love the whole sober curious movement, I mean, and it’s everywhere, right? Like New York Times, Good Morning America. Everybody’s talking about it.
Yeah. But also, the idea is that to make it more approachable, but also, like, try. Try to see, like, longer period of time, alcohol-free. I recommend 100 days. That’s what I started with. And then, like, see, because that way you’ll see that you can socialize and you can go on vacation and you can watch TV, and after a hard day of work, you can try a different coping mechanism.
And like, at the end of that time, you feel better when you know. I have a group of women who are all you know in the process of going alcohol-free, and just the fact that you know, one of them said, Oh my god, I woke up with like a cold, the flu, of migraine. I didn’t sleep. I can’t believe I used to feel this way every day, I can’t believe how shitty I felt and like I’m having one day of it and I’m just like, now I know what healthy feels like.
Dr. Nzinga Harrison 16:30
Yeah, I love that so, so, so much. And this is like you said, you recommend 100 days, which I love, 100 days because I didn’t think I’d be able to go on the girls trip or live and all this kind of stuff. The book is called, 6 Mind Changing Conversations, and there are actually scripts in the book like, how to have this conversation. And one of them is like, Okay, we’re going on a girls trip, and either I’m choosing not to drink, or I have a friend who’s drinking. I’m worried about, how do we talk about it? Before we go like, what is your plan for when you find yourself in a situation you’re in 100 days not drinking? What’s your plan for when you go out to dinner? Yeah, and the server has great intentions and has been instructed by their boss to offer everyone a drink, and you’re going to say that’s where they make their profit margin, right? That’s where they make their profit margin, right? I was at a business dinner, and it started out with drinks, and so those the server came around and was taking everybody’s drink, and everybody was ordering an alcohol drink, and that was back when I was still drinking, but me and my husband decided to stop drinking. It’s been like, a year now.
Casey McGuire Davidson 17:41
Oh my god. The last time we talked, you were like, I don’t drink a lot, but I do.
Dr. Nzinga Harrison 17:46
I barely, I barely drink. And then, I was like, why am I even spending money? But that’s amazing, because, yeah, so he was actually the one. He was like, I’m going to stop drinking. I was like, Okay, I’ll stop drinking. So, we haven’t drink for like a year, we’re, like, totally into nonalcoholic cocktails.
Casey McGuire Davidson 18:03
Oh, my god, me too. Oh, my God, I love nonalcoholic beer. That’s my jam.
Dr. Nzinga Harrison 18:07
Oh, I hate beer.
So, I love nonalcoholic beer for other people. But for, like, the book launch, we did a total nonalcoholic spread. So, we had nonalcoholic Heineken, nonalcoholic, Corona, nonalcoholic. Sparkling wine was like, sparkling wine was my jam. So now nonalcoholic, sparkling wine is my jam. I love it and cocktails.
Anyway, before that, I was at this business dinner. Everybody’s ordering a drink, so I was going to get a Prosecco. That’s what I used to drink. But the person before me, so it’s like, 12 of us. We’re on, like, Person number 7. I’m like, number 8. 6 people order alcohol drink. Person number 7 says, Do you have anything nonalcoholic? Yes. Like, damn, and the bar happened to have nonalcoholic cocktail. And they’re like, yeah, we can do a blah, blah, blah. And he was like, I’ll take that. And I was like, I was planning on ordering a Prosecco, but I’m going to go for the nonalcoholic drink he just ordered. And do you know of the next 5 people, 3 people chose to do a nonalcoholic drink, and two other people changed their order.
Casey McGuire Davidson 19:26
They didn’t from alcoholic to nonalcoholic, like he just unwittingly, yep, made it okay when we wasn’t, like, whispering about, like, bring me this so people think I’m still drinking or none of that.
Dr. Nzinga Harrison 19:31
Just was like, Do you have anything not alcoholic? And I was like, Uh, I’ve just seen you role model how I plan to be going forward. It was incredible. So, back to sober curious is like, Hello Someday podcast, all of the people in New York Times, all of the people on the web that are like, Yeah, I just decided to stop drinking. You’re making it safe for somebody else to say, I’m going to try it like I love it so much.
Casey McGuire Davidson 19:59
It’s become such a thing with like, Dry January, Dry July, like this, the younger generation not drinking as much, like there’s a zero proof cocktail menu, or a nonalcoholic beer that’s actually good, that’s not crap, right, on almost every single menu. And I mean, when I quit drinking 8 years ago, I actually tried for the first time 11 years ago, that was not a thing.
Dr. Nzinga Harrison 20:26
Yeah, it was not a thing. It was not a thing. And it’s so good. I mean, I talk about the cultural pressures, yes, right? I love that faith, and this is one of them. I mean, we basically, you and I are the same age.
Casey McGuire Davidson 20:45
We were just talking about that.
Dr. Nzinga Harrison 20:48
We’re the same age. And when we grew up, I think we pretty much started getting programmed with just wait until you can get smashed when you turn when you get to high school. In elementary school, we’re seeing that on TV, right? And so, you just grow up with this concept that there is no life without alcohol, and there’s amazing life, yeah, without alcohol. So, and for some people, there’s amazing life with alcohol. Before a lot of people, there’s not amazing life with alcohol. So how do we create space?
Casey McGuire Davidson 21:20
Yeah, and the way it works, too, from my experiences, it starts very innocuous, and it starts because of your culture. And, you know, although the first time I got drunk, I like, blacked out and, but that was, I was doing that on purpose for some I mean, I didn’t want to black out, but I wanted to get super drunk, because, you know, opportunity, but you know, when I was growing up, it was like there was a bottle of wine on dinner, the dinner table every night, because that’s what adult strength My grandparents had, like happy hour before dinner. And we’re going to talk about all the risk factors nobody in my immediate family, meaning, like parents, grandparents, sibling, whatever, struggles with alcohol. I definitely did, but you know, the underlying stuff of like anxiety, or, you know, various things we’re going to talk about.
But also, when I went to college, I joined the women’s rugby team, and I had a very big keg college culture and the rugby team was, like, a four year crash course on problematic binge drinking and blacking out and throwing up and like, that was like. I was like, Oh, this is what we do, right? That’s where you talk about culture to everyone I knew, binge Strang, you know, all the time it was like the purpose of drinking was to get so drunk that anything could happen. Yeah, and you know it, it does skew the way your brain works. You know it does.
Dr. Nzinga Harrison 22:58
It does. And you mentioned nobody else in your family has struggled with alcohol.
I imagine someone else in your family has struggled with anxiety or depression or cigarettes or another societal pot or suicidal thoughts or food addiction or work addiction, right? Like, all of these are running through the same pathways in our brains, and so that you experienced anxiety yourself made you particularly vulnerable yes to that kid culture in college, right?
Casey McGuire Davidson 23:34
Okay, I want to dive into the conversations and the factors, but the one thing I also wanted to ask when we talk about that 75% recovery rate is everyone talks about relapse, and I absolutely love that you talk about that relapse is not a part of the illness. God, throw it in, 5% of people with substance use disorder recover and return to use in the first couple months, in the first year. Where’s the tipping point? Can you like, teach us all of that stuff?
Dr. Nzinga Harrison 24:10
Totally. 100%. So, I’m going to go a little medical here. And what I want people to know about the book is, yes, I’m a doctor. This is not a textbook. I wrote this book so good like a conversation, or at least, that was my goal, right? But I’m going to get a little textbooky Dray or for just a minute facts, right?
Casey McGuire Davidson 24:28
That’s what you talk about, versus reality totally.
Dr. Nzinga Harrison 24:32
And so, in medicine, when we talk about chronic conditions, we talk about relapse and remission when you get diagnosed, that is because you meet diagnostic criteria for fill in the blank, diabetes, high blood pressure, alcohol use disorder, if we’re talking about alcohol addiction, when you go into remission, that means your symptoms have come down. Down below the threshold that meets diagnostic criteria for active illness. When you have a relapse, that means symptoms of the illness have come back above that threshold. We talk about like that person relapsed. People do not relapse. Illnesses relapse. We talk about you had one drink. That’s a relapse. One drink does not meet diagnostic criteria. That is not a relapse, right? And so, what is so critically important, when people say relapse is part of the disease, I hate it. Throw it in the trash.
Casey McGuire Davidson 25:40
100% because that, like, plants that seed. When you talk about planting the seed, like there’s no other totally and you’re just like, like, it’s inevitable, yeah, yeah, like, it’s inevitable.
Dr. Nzinga Harrison 25:51
That would be like, if I diagnosed you with breast cancer, and I said, I’m diagnosing you with breast cancer, we’re going to do everything we can do to get you in remission, 75% chance that you’re going to recover, but relapse is part of the disease. I just told you like, no matter what you do, cancer is coming back. That is awful, and it’s not even true, right? That’s not even true, okay?
So, what we have to say instead is, you know what, I’m really concerned about your alcohol use it meets diagnostic criteria for alcohol use disorder, mild, moderate or severe, right? You have 75% chance of recovery from this illness, and based on my medical knowledge, these are the things we can do to give you the best chance to be in that 75% now there is a chance of relapse with this illness, and what relapse means is these are the diagnostic criteria, and the risk factors that drive your risk for relapse are xx, xx and x. So, we’re going to make a plan for xx, x and x, so that hopefully relapse does not become part of your illness process. Yeah, that’s the way to have the conversation.
Casey McGuire Davidson 27:07
Yeah, absolutely. And so let’s first talk about what are the things that will say you’ve stopped drinking, say that previously, you met the diagnostic criteria, or you didn’t. You did curious, like, that’s right, but like you stopped drinking, your intention is to not go back to it because you feel like shit and it pick up all your thoughts and whatever it is, what are the things that you would do to make sure that you’re in that 75%?
Dr. Nzinga Harrison 27:40
The first thing is understanding your risk, right? And so, this book is divided into 6 chapters, and each one of the chapters is dedicated to a certain type of risk.
So, you can think of this framework in the first bucket, for any chronic condition, there are biological reasons why you develop it. There are psychological reasons why you develop it. There are environmental reasons. And the environment splits into two. That’s the cultural environment as well as the physical environment. You are born into a biological set of risk factors. That’s your DNA, right? So, people don’t know, 40 to 60% of your risk of developing addiction is coded in your DNA. The day you’re born.
Casey McGuire Davidson 28:23
This is that because of family history, or because people in your family have also had those biological things, like, it’s, is it passed down? Or you have it is similar?
Dr. Nzinga Harrison 28:36
Okay, it is DNA that is passed down to you, just like DNA for high blood pressure is passed down to you, DNA for cholesterol is passed down to you.
Okay, so got it.
40 to 60% of your risk for developing an addiction coded in your DNA, higher than diabetes, higher than asthma, higher than high blood pressure, okay, born with it. But that means 60 to 40% because we add up to 100 is psychological and environmental. You are also born into early childhood experiences, psychological risk factors.
You are also born into a cultural and physical environment. So, I call that inherited biological risk factors. That’s your DNA. Inherited psychological risk factors. That’s your childhood inherited environmental risk factors. That’s the culture and physical environment you grow up in. That’s 123, repeat those three again as you become an adolescent, young adult, older, adult, whatever’s in the middle, just adult. I think me and you right now are just adults. Right when you grow into that, you start to acquire things, things start to happen to you in life that can also be risk factors.
So biologically, maybe you get a car accident and break a bunch of bones. That’s a biological risk factor. Maybe a doctor writes you a prescription for opioids, that’s a biological risk factor. For people who are alcohol. Sober curious, maybe a doctor writes you a prescription for Xanax. Yeah, and Xanax is alcohol and pill form works on the exact same receptor in the brain, right? That’s a biological risk factor. Psychologically, you develop the stress of racism, the stress of discrimination, the stress of gender discrimination, the stress of being the only woman in the workplace, the stress of being the only mom who’s not a stay at home mom, or the only mom who is a stay at home mom in your high needs kids, or high needs, or divorce, right?
Casey McGuire Davidson
Hi there. If you’re listening to this episode, and have been trying to take a break from drinking, but keep starting and stopping and starting again, I want to invite you to take a look at my on demand coaching course, The Sobriety Starter Kit®.
The Sobriety Starter Kit® is an online self study sober coaching course that will help you quit drinking and build a life you love without alcohol without white knuckling it or hating the process. The course includes the exact step by step coaching framework I work through with my private coaching clients, but at a much more affordable price than one on one coaching. And the sobriety starter kit is ready, waiting and available to support you anytime you need it. And when it fits into your schedule. You don’t need to work your life around group meetings or classes at a specific day or time.
This course is not a 30 day challenge, or a one day at a time approach. Instead, it’s a step by step formula for changing your relationship with alcohol. The course will help you turn the decision to stop drinking, from your worst case scenario to the best decision of your life.
You will sleep better and have more energy, you’ll look better and feel better. You’ll have more patience and less anxiety. And with my approach, you won’t feel deprived or isolated in the process. So if you’re interested in learning more about all the details, please go to www.sobrietystarterkit.com. You can start at any time and I would love to see you in the course
Casey McGuire Davidson 30:27
Whatever relationship, abusive relationships, all of those things, environmentally, cultural environment.
Dr. Nzinga Harrison 30:35
You go to a school and join the rugby team, and it’s the keg culture, physical environment you live in, a place where all your needs are not being met, right? And so that biological, psychological, environmental repeats again. These are the six buckets.
So, your question was, how do you know what to look for? First is knowing what you have in each bucket. So inherited, biological, do your addiction, family tree? Have the conversations. There’s a script in the book to help you have the conversation. Inherited, psychological, your aces, your adverse childhood experiences. Know what they are, put a plan in place to start dealing with the impact they are still having on you environment. You
Casey McGuire Davidson 31:23
give a just a couple example of aces, in case someone doesn’t know what those are, totally and also, you can Google aces adverse childhood experiences, and you’ll find it. I do not recommend that you just Google it and take it without having a support system in place for yourself.
Dr. Nzinga Harrison 31:29
And the book goes through this, but aces are for example, did you experience emotional abuse as a child? Did you experience physical abuse as a child? Did you have a parent who had a mental health condition or addiction? Did you have a parent who left the house because of divorce? Did you have a parent who was incarcerated, right?
And so, there are 10, there are 10 questions. And if you get a one for every yes question, if you have a score for higher your risk for developing all sorts of chronic conditions in adulthood, including addiction, premature birth, obesity, cigarette smoking, premature. I mean, asthma, HIV, cancer, like, literally, all kinds of things are associated with this.
My aces score is five. My inherited biological risk is probably closer to that 60% because I have addiction, both on my mom’s side and on my dad’s side to different substances, right? That allows me to understand my risk, but also allows me to start having a conversation with my kids about their risk. And then same thing, bio, biological, psychological, environmental.
When you grow up so Casey, what is your biological risk? If you’ve decided you don’t want to drink again, then I need to look at how much biological risk we have, because that means I have to do even more with your environment to try to undermine that risk. What’s your aces score? We need to address all those experiences that you had. What environment are you currently in? What are the people, places, emotions, physical sensations. How are you going to talk to your friends? What are you going to say at work when your boss says, Come to happy hour, right? Like, we had to make a plan for all those risk factors to increase the chance that you’re in the 75%.
Casey McGuire Davidson 33:40
Yeah.
Dr. Nzinga Harrison 33:41
Yeah, that was the longest answer.
Casey McGuire Davidson 33:42
I love it. It’s so important and that like that last piece, other than the hope and the curiosity, is a lot of the work that I do is okay, you want to stop drinking, but you keep going back to it. Like, what is your home environment like? What conversations have you had? How can you have them without it being scary or getting pushed back? Like, how do you go to dinner with your spouse? What do you say at happier? How do you go on a business trip, all of those things? Because for me, it was one, the fear that life would suck and everything that goes how will I relax? How will I have fun? But it’s my favorite thing in the world, but it’s my only reward. Yada yada yada. But then, how, literally, how do I go on a double date with another couple to celebrate something and tell them I’m not drinking or not, dive over the table and, like, grab the drink, right? Yeah, and, like, just that block and tackling in a really practical way is like another step that is you have to do, you know, have to do it.
Dr. Nzinga Harrison 34:57
And we literally go through scenarios in the book for how to do this, and what I say is, do you know why a race car driver can take that curve at 200 miles per hour? It’s because they’ve practiced, yeah. Do you know why they can safely get out of a crash? It’s because they’ve been in a simulator. Why Captain Sully, could land that plane on the Hudson River is because he had practiced right? And so, you don’t want to be in a situation and have to figure it out. You conjure up those situations in your brain in advance, and you practice, okay, this is what I’m going to do if, this is what I’m going to do if And then you also practice if I find myself in a situation that I haven’t practiced. This is my go-to, yeah, that I’m going to do. And the more you do those reps, it gets easier and easier and easier to say I’m not drinking. And people are like, what? And you’re like, Oh, you think that’s weird. I’m getting the best sleep I was ever getting when I was drinking.
Casey McGuire Davidson 36:00
Yes, yeah. I love that you already have your one liner queued up.
Oh, yeah. And you know what you’re going to order, and you’ve told someone in advance you’re not drinking. You ask someone with you for support, and that’s right, all, all the things, all the things.
Dr. Nzinga Harrison 36:23
So, you talk about the 75% success rate, which, by the way, I’m just going to keep saying some people over and over, over 30 more times before we finish.
Casey McGuire Davidson 36:27
Yes, but you talk about it in the context of the impact of long term treatment for addiction, and obviously that doesn’t only mean inpatient rehab. That’s right.
So, tell me what the different factors are in terms of what you think of when you think of long term treatment for addict. Because for some people, that’s scary, right?
Like, I’m going to attend 12 step meetings for the rest of my life, right? And talk about what a horrible person I am, but also surround myself with people who are not drinking and right label myself. So, what are the sort of tiers or options, or any of that?
Dr. Nzinga Harrison 37:03
Yeah, so, um, I want to think broader. I want the word treatment to people to mean, like your broader action plan. And so, I’m going to talk about diabetes because I always do, because I think it’s easy for people to grasp. And by the way, there’s no stigma about that, and there’s no stigma. That’s exactly what I talk about.
Casey McGuire Davidson 37:25
It’s like, nobody’s like, oh my god, yeah, right. It’s just a condition you treat. It’s like, I take medication for anxiety, and I also try to work out, and I also totally all the things, right?
Dr. Nzinga Harrison 37:39
Totally, right. And so, what if we thought the treatment for diabetes, for a person that had diabetes so severe, their blood sugar got so high, they went into a coma, they had to go in the ICU. They went in the ICU for five days. And we were like, All right, that’s it. That’s kind of like the concept of detox, like, that’s it. No, if we just get them out of the coma and send them right back out to the exact same set of circumstances with no medication, no support, no understanding of the illness, they’re going to be back in a coma, right?
What if we said, Okay, we got you out of the coma, we took you out of ICU, we put you on the inpatient floor for a week. Got your blood sugar totally normal, then we discharged you. Good luck living with diabetes. Nothing else, right? Diabetes is coming back. What if we said for the rest of your life, every single day you have to come to the doctor and get an insulin shot? That would be like diabetes is coming back, because nobody can come back to the doctor every single day. That’s not how we think about it. We think about it like, you go in, you get stabilized, you come out, you get connected to some doctor that you can meet with in the beginning frequently, until you figure out what’s going on. And then, as you stabilize and figure it out. You know what your warning signs are for when you need to get back? That’s the way I want people to think about this.
So sober curious, try it. Stop drinking. Whoa. Felt the best you ever felt in your life. Make the decision, I’m not going to go back to drinking, either at all or definitely not to the level where I was drinking before. Get your support in place. Get your medication if you need it. Get your therapy to address those adverse childhood experiences. Get your stress your support system to get those stressors down. Get a new job, find a new spouse, whatever, whatever you have to do right? Do all of those things. Know what your early warning signs are. I am doing great. I don’t need to see you every month. I’ll see you every two months. I don’t need to see you every two months. I’ll see you every three months. I don’t need to schedule an appointment with you, but if I notice x, x and x, I’ll reach out to you. And so, that’s what I mean by long term treatment. The same way you have your primary care doctor.
You should have your person, whatever role that is that you know your early warning signs. They know your early warning signs. You can get in with them before your symptoms cross that threshold to equal a relapse now.
Casey McGuire Davidson 40:19
I love that, and that is so true in my experience, not just for myself, but for so many of my coaching clients. When I stopped drinking, I had an online group that everybody was sort of on the path to not drinking. So helpful. A lot of people were 3 and 4 years on, who were giving support and encouragement and tips, and I had a sober coach that I worked with. I emailed her like every single day. We had phone calls every once in a while. And then, when I was 60 days sober, I joined Hip Sobriety School, which was like this online course, slash group, slash whatever, with Holly Whitaker, who wrote, quit like a woman, yeah, today. And so, that was reinforcement. And then, I started seeing a therapist once a week, and I got on some medication for anxiety or mood disorder. And, like, that was my first year, and it wasn’t a, like, a horrible thing. It was like, oh my god, I’m finally getting healthy. I’m finally not waking up with a hangover, hating myself, feeling strung out with anxiety, craving alcohol, worrying about it like this was, I worked out, you know, all the things, and then after a year, I didn’t need to see my therapist anymore.
And after a year, I stopped emailing my coach 5 days a week. But I had also, everybody knew I didn’t drink. It had become part of my identity. Yep, I felt good about myself. I had my sober friends, like good, good friends. And I also stayed in touch with my group. I knew that if I felt really anxious or panicked or whatever I needed to, like, deal with it right away. You know, like and trust me, in eight years, I’ve gone back to my therapist, who knows that I don’t drink, and I keep myself in a good mental health place, so that I don’t go back to drinking or something else, right? But I don’t. I haven’t seen my therapist in 2 years because I’m good.
Dr. Nzinga Harrison 42:31
That’s right. And, you know, so I love so much. We talk about this in the book the magic formula, and I say, what I love about the magic formula is that it’s not magic. It is just your collection of things, yes, that keep you healthy as you are defining healthy.
And I love that journey you just shared with us, Casey, because that collection of things has to change over time, because your life is changing over time, and the ideas like match your magic formula to what’s happening for you right now.
And so, I would say, people think of treatment and they’re like, Oh God, I got to be an AA every day for the rest of my life, or I’m going to be in a halfway house, or I got to live in residential treatment. I would wager to say, Casey, that part of your treatment is this? Hello, Someday podcast.
Casey McGuire Davidson 43:23
Oh, god yes.
Dr. Nzinga Harrison 43:24
I mean, one of your early warning signs would be like, if you could not bring yourself for I’m just going to say three weeks is probably shorter to not make this podcast, you would be like, This is a warning sign, and I need to bring in supports.
Casey McGuire Davidson 43:43
Yeah, yeah. I mean, I tell people that all the time. They were like, do you think it would be easier for you to go back to drinking if you weren’t talking to people every day in a group that you’re running doing the podcast? And I’m like, hell yes, because first of all, helping people in early sobriety reminds me how much it sucks, like, how much drinking is not what we see on TV. And you talk about that too, how glamorized it is, and how harmless it is, and all those stuff. But, like, also, I get free therapy. Like, I’m talking to you, I talk to other people. I reach out to people about the shit that I need. Like, I’m like, Okay, talk to me about marriage, talk to me about, like, perfectionism, talk to me about imposter syndrome. But, like, that’s the ongoing work, and it’s great. It makes me happy.
Okay, I’m going to ask you a totally off topic question, okay, because I’m just curious, and then we’re going to go back to it.
So, this is going to sound so stupid that I just want to know. So, I went to my doctor recently, right? And I looked through, you know, they give you the report on all your numbers and blah blah blah blah blah and on there. I forget what there was, but it was like anxiety, blah blah blah blah blah. And they, then, they say. Said alcohol use disorder severe, and maybe they said in remission. I don’t even remember, but I read that, and I was like, Can I get that downgraded model? Like, I was kind of pissed that was there, because I was like, Dude, do you know how many of your clients patients drink a fuck load? I haven’t had a drink in 8 and a half years. Why? The Why’s, the shit on my chart? Is that terrible?
Dr. Nzinga Harrison 45:26
Um, is your reaction terrible? Is it terrible that you’re in that, it’s in your chart?
Casey McGuire Davidson 45:32
Well, reaction is not. I’m wondering about my reaction. I actually told my girlfriends. Yes, sober, I’m like, first. Why does this bother me? Because the anxiety thing doesn’t bother me. So, like, clearly that, although I still struggle with anxiety and I don’t struggle with alcohol anymore, but B, I was like, it’s inaccurate.
Dr. Nzinga Harrison 45:55
Well, yeah, it seemed to me to be a present tense. Yeah, it is legitimately an inaccurate diagnosis.
Casey McGuire Davidson 46:00
Okay, tell me about that. Go, like, seriously. Like, I want to go back to my doctor and be like, I’d like you to change that.
Dr. Nzinga Harrison 46:06
You can and I’ll give you exactly what you can ask them to.
Casey McGuire Davidson 46:09
Oh, please. Okay, what’s what? Tell me why it’s inaccurate.
Dr. Nzinga Harrison 46:14
Yeah, it’s inaccurate because we diagnose alcohol use disorder, mild, moderate, severe, in early remission or in sustained remission. Okay? Those are 5 mutually exclusive diagnosis. So, we have 10 diagnostic criteria for alcohol use disorder. If you only meet one, you do not have alcohol use disorder. You have risky alcohol use. We should be trying to prevent you from transitioning. If you have 2-3 of those 10 criteria, you have alcohol use disorder mild. If you have 4-5, you have moderate. If you have 6+, you have severe. If you have not met diagnostic criteria for 3 months, you have alcohol use disorder in early remission. If you have not met diagnostic criteria. And remember, this is not just taking a drink. This is meeting, yeah, those 10 diagnostic criteria for 12 months you have alcohol use disorder in full sustained remission.
And so, what happens? This is like everybody’s chart that I always ever see you come in 8 years ago, you have alcohol use disorder severe. You get 3 months, nobody updates the diagnosis to early, right? You get a year. Nobody updates the diagnosis to full sustained remission. And he’s correct to keep that alcohol use disorder diagnosis on your chart, because we should be practicing prevention right now, right like I know if your anxiety is not controlled, that’s giving me risk. I know if your blood sugar goes low, that’s giving me risk, that kind of stuff, but it should update it to alcohol use disorder in full sustained remission. I think your reaction, part of it feels like undermining all the hard work you’ve done for eight years, yeah, which is true. Second is communicating something about you diagnostically. That’s not true. That never feels good, yeah. Third, I think about it like cancer, if you had cancer and then your cancer went into remission. When you read your chart, you want to be reminded that your cancer is in remission, yeah, so I’m totally validating your reaction. And what you can go back to the doctor and say, so I’m actually going to give you the code, okay? Because alcohol use disorder, ICD 10, we use numbers to give the code is 10.2 that’s what your doctor currently has in your chart, okay? And your doctor just needs to choose 10.21, assist. All right, disorder in remission.
Casey McGuire Davidson 48:58
All right, I am totally going to do that the next.
Dr. Nzinga Harrison 49:02
Yeah, and have a conversation about why it matters.
Casey McGuire Davidson 49:07
Like I’m eight years not drinking, it’s important to communicate that.
Dr. Nzinga Harrison 49:11
Yeah, totally, I’m with you. All right. I love it.
Casey McGuire Davidson 49:13
Okay, I see. I’m glad I asked. I get all the good information.
So, I have to tell you when I read the title of your book, 6 Mind Changing Conversations That Could Save A Life. I thought it was going to be like I’ve seen in some other books, like a mall, you know, like a compilation of a client’s story, right? Like, okay, this is, you know, Sophie and she XYZ, and you know what I mean? Because I’ve seen that before, and I love those two.
But what I loved about this was, it was like scripts for conversations you can have, not only about yourself, not only about how people can support you. But like, how do you bring it up with your kids? How do you have the if they are, like, so good, like, elementary school, middle school, higher. I mean, tell us what the conversations are so people can kind of dive in, because this is the practical shit that people need.
Dr. Nzinga Harrison 50:18
That’s right, right, that’s right, I tried to write a super practical book that everybody could see themselves in, whether they feel like addiction has never been part of their lives, somebody else’s life, whether they’re curious this sort of thing.
So, the first. The conversations follow that framework that I told you, inherited biological, psychological, environmental and acquired.
So, in inherited biological, it’s how to have a conversation with your family about how addiction has affected our family, and it helps you in making that addiction tree. And that’s not easy, right? Like a lot of families, this is a taboo subject that nobody is going to bring up. And so like, how do you have that conversation with your family about what our risk is? DNA wise as a family, inherited psychological is. How do you have one understand your own aces score adverse childhood experiences? How do you have that conversation with someone to support you in thinking about all those harmful experiences that you had as a child and how they are still affecting you today. Inherited environmental is how do you have the conversation around how the culture you grew up in and the physical environment you grew up in is still affecting your choices today. Yeah, affecting your life experience today.
And then, when you come into acquired biological you had an injury or developed an illness, or a doctor wrote a prescription. How do you have a conversation with your doctor about your risk for addiction and the risk of the prescription they’re writing you, and how you put a safety plan around that prescription. Yeah, inherited psychological is about positive childhood experiences which nobody ever talks about, but which totally like negate adverse childhood experiences. And so, it’s like, how do you have one. How do you have the conversation with yourself to understand your own emotions, and then how do you talk about those and have conversations with friends? And then also, how do you talk about the discrimination you’ve experienced and how that drive your risk? And then inherited environmentalist, how do you have the conversation about what my physical environment is today and how and why I need to change that?
And so, it just go, Oh, I’m sorry I didn’t, I think I didn’t mention the script with your kids, which you mentioned, which is every single age, yeah, like I started talking to my kids when they were three, and now they know how to talk about addiction with their friends.
Casey McGuire Davidson 53:03
Oh my gosh, like my kids totally know, because my son was eight when I quit, yeah, and my daughter was two, and of course, in the beginning, I didn’t talk about a ton of stuff with them. I was just like, Yeah, I haven’t had a I don’t my son, of course, I had a bad day. He’s a you know, he was like, Oh, mom, want me to get you a glass of wine. I was like, but they know, right, that’s mom. I mean, I can’t tell you how many women have said that the kids go in and tell me about your mom and like, what’s her favorite drink? And it’s like, gin and tonic. And they’re right. But, you know, knew that, and then, of course, because when I had gone further, like my son and my husband got me for my 1000 days, alcohol free, I still have it in my office right behind me. They got me a big glass jar and put 1000 like little marbles in it, and it just made me so happy and just proud. And it was amazing. It makes me a cake every year on my sober bursary with, like, I remember, they did the number five with all strawberries and blueberries.
So, they’re pretty great. But, like, I’ve had my daughter on my podcast when she was nine, talking about, like, how we talk about alcohol and what she knows about it. And you know, so I love that you did that. Because so many women, they’re like, What do I say in a way that’s helpful and they understand, but not like, oh my god, Bob was a, you know, drunk, or whatever it is, because, you know, it’s not that it’s mom decided not to drink, and that’s super awesome. And that is super awesome, right?
Dr. Nzinga Harrison 54:48
Yeah, and, and it’s super awesome. And you also can make the decision not to drink if you choose to make that decision at some point, yeah, you have a role model that you’ve seen. Lives an amazing life that way, right?
So, people often talk about addiction as a family illness, community illness, which is absolutely true. So is recovery like when you think about those positive childhood experiences. And what we talk about in the book is that all of these work as adults also. So even if you didn’t have them as a child, you can put them in place as an adult. Part of that is, were you able to talk about your emotions? Yep. Did you have community traditions? Did you have somebody you knew would stand up for you and so like your husband and your son giving you a jar of 1000 marbles on the 1,000th day, you already know when you go to a restaurant, and the service says, Can I get you a drink? And you’re like, I don’t drink. And they’re like, what your husband and your son are going to be? Like, listen.
Casey McGuire Davidson 55:49
Yeah, right. Yeah. They’re just like, yeah, no. And my husband still drinks, you know, and it’s not a thing, but he’s super proud of me for not drinking, and I love it. So, no, in the beginning he didn’t want me to stop drinking, right? He wanted me not to, like, pass out on the couch. You know, it was, like, part of our thing, but like, that’s the evolution that you go through, and you have a new normal, and the new normal is great, because mom never passes out on the couch, and dad can’t wake her up and she’s not hungover and pissed off and whatever it is, right, right, right, yeah.
So, all right, I love this so much you go through, like the coping mechanisms and mental health and policy and personal like all the good stuff that you need to know. I just have we not touched on any misconceptions or myths that you’ve addressed in your book. Like, I just want to be like, we’re not going to go through them all. But here’s the things you think you know that are not true.
Dr. Nzinga Harrison 56:56
Um, the things you think you know that are not true.
One, people don’t get better, because 75% of people recover. We said we’re going to keep saying it.
Two, it’s everybody else. It’s all of us, yeah.
Three, you have to be drunk in the gutter, yeah, or to be a problem. There is, I would love to talk about the cage question. Do that please.
Second, please, please. So, what I’m really, really, really advocating for is the same way for breast cancer. We want everybody to do their monthly breast exam, because the earlier you catch a lump, the better chance we have for sustained remission, no relapse. The same is true.
So, I tell people, if you ask yourself, either about yourself or about somebody you care about, should I be worried? The answer is yes, yeah. It doesn’t mean you have a diagnosis. I don’t care if you get a diagnosis or not, but if you say, Should I The answer is yes. And so, here’s a scale that I can give you. It’s called the cage.
See, have you ever thought you should cut back If yes, give yourself one point A. Have you ever been annoyed when somebody else mentioned you’re drinking to you? Give yourself a point. Have you ever felt guilty because drinking prevented you from doing something you plan to do, or you said I’m not going to drink today, and you still drunk like if you ever felt guilty over alcohol and E is for eye opener, have you ever needed to drink first thing in the morning or thought about drinking like it’s the first thing on your mind when you wake up? Those four questions are called the cage. If you answer yes to one of those questions, there is 77% chance that you have an alcohol use disorder, whether that’s mild, moderate or severe, even the 23% that don’t have an alcohol use disorder have an opportunity to not develop an alcohol use disorder.
So, ask yourself those questions. And this is the other myth that I want to bust, is that it’s dangerous to ask for support. It’s not dangerous to ask for support. It’s dangerous not to ask for support. There are so many ways. So, if you’re thinking to yourself, I wonder, give yourself the cage or give, you know, take the cage on behalf of somebody you’re concerned about and ask for support. It is the safest way.
Casey McGuire Davidson 59:33
Don’t, ignore the lump. Don’t, don’t. And you know, there are different ways to get support, and we can talk about all that, and I’ve talked about it in previous episodes. But it doesn’t mean you have to make a huge declaration that’s right to anyone there is support available that is, you know, completely private, completely confidential, whatever it is. Um, yeah, I was the first 3 out of those 4.
Yeah, yeah. And, like, drink first thing in the morning, no, unless you go out to brunch, right? Like, I love how we like switch what we do, yeah, exactly.
Dr. Nzinga Harrison 1:00:12
I mean, a mimosa or bloody Berry, like, that’s just totally run straight, right? Totally.
I mean, I was on the plane the other day, because I think I’m on a plane every other day, but I was on a plane the other day, and I was on a 6am flight, and we were leaving on time, so it was 5:45am and the flight attendant came around and said, Can I get you anything to drink before we take off? And this person said, I’ll take a red wine at 5:45am and I don’t jump in strangers businesses that are seated across the aisle from me. But I thought to myself, Man, I wish it was safe for me to jump across the aisle and just say, I’m just saying, if you need any support here some ways, like if you’re worried about yourself, yeah? Because at 5:45am that’s an eye opener.
Casey McGuire Davidson 1:01:01
Yeah, yeah, totally. And I always say to people, because they’re like, Oh, my God, all my friends drink, but like, nobody else is worried about it, blah, blah, blah. And I was like, dude, anyone who is drinking with you the way you’re drinking, they wake up at 3am worried about their alcohol consumption. There is zero chance, like it just doesn’t happen. You guys are just not talking about it.
Dr. Nzinga Harrison 1:01:25
Yeah, to make it safe to have the conversation.
Casey McGuire Davidson 1:01:29
Yeah, yeah. Okay, one thing we talked about before we jumped on here, and I know I got to let you go, is we both said that we don’t love the term alcoholic. Can you tell me why?
Dr. Nzinga Harrison 1:01:39
Yeah, I hate the term “ic” for anything.
So, I hate diabetic. I hate schizophrenic. I hate alcoholic, I hate asthmatic, and the reason is because that is not who you are.
You are not an alcoholic. You may be a person that struggles with alcohol use you may be a person that has a diagnosis of alcohol use disorder. You may be a person that just doesn’t want to drink, but the struggle you have with alcohol will never, ever be the most important thing about you. It will never, ever be the thing that defines you.
It’s one thing that you’re going through, and so I just always start with the person first, to remind us that, first and foremost, you are a person. And then second, we can use you know, words to say what your current life experience is, but don’t take on that definition.
Casey McGuire Davidson 1:02:45
Yeah, yeah. And don’t force that definition on somebody else, on anybody else, like people use it so casually. Be like, Hey, oh my god, her dad was such an alcoholic. And I’m like, I hate he also pisses me out well, mostly, unless they are in a 12 step program, and they self-identify, and that is fantastic, whatever. But like, especially for people who have never struggled with addiction, when they are casually labeling somebody else, and I’m just like, WTF.
Dr. Nzinga Harrison 1:03:14
Like, 100% stfu, how about that?
Casey McGuire Davidson 1:03:18
Yes, yes, yes. I believe I have, like, occasionally said that in a much nicer way, be like, dude, uncool. Like, so and you don’t know what the fuck you’re talking. Yeah, so uncool.
So, okay, one more, last one. It’s like rapid fire when the hell are the medical directives information going to change? I mean, I know there’s huge lobbying stuff, but like the American Cancer Society finally said, What 3, 4 years ago, that no amount of alcohol is zero risk factor for cancer, which they had known for fucking ever.
But like, Ireland is putting labels on every single wine bottle and beer bottle saying, like, alcohol causes liver, you know, severe liver, liver disease. Alcohol causes cancer, same way as tobacco. U.S., I’m not hearing shit.
Dr. Nzinga Harrison 1:04:18
Yeah, it’s 2 things.
So, 1. I forget what the statistic is, but something like, it takes 22 years for medical practice to change, which is crazy, so we’re in the midst of it, but it’s very slow.
- Money talks and alcohol lobby is so rich, and it is so ingrained in our culture, which I talk about in the book, and that’s the reason why it’s so slow.
But listen, young people are the future. Young people are like, totally our hope, because they’re like, it’s cool to not drink, yeah. End drinking, you know? And so, it will come, but it is going to be so slow. So, that’s why.
We can’t depend on the external forces. We have to start with these conversations just like this, yeah, and this book and just let it broadcast into people’s individual minds.
Casey McGuire Davidson 1:05:12
Yeah, it is so slow. All right, I love talking to you.
I love your book. It’s called Un-Addiction. You guys should totally pick it up.
Your podcast is called Un-Addiction, and tell us where else people should look for you, find you.
Dr. Nzinga Harrison 1:05:25
Yeah. So, you can find me on Instagram, Facebook, formerly known as Twitter, now called X threads and LinkedIn @NzingaMD or Nzinga Harrison MD.
I co-founded this company, Eleanor Health, which I’m so proud of so please check out eleanorhealth.com. And then, the book is in print, audio and digital everywhere, in stores, online. Do you?
Casey McGuire Davidson 1:05:49
Do you read the audio?
Dr. Nzinga Harrison 1:05:50
I read the audio.
Casey McGuire Davidson 1:05:51
I love it.
Dr. Nzinga Harrison 1:05:52
I had to audition, I had to audition to narrow the audio.
Casey McGuire Davidson 1:05:59
But I like, you’re like, of a fucking podcaster. I could do this, and it was. So, it was awesome.
Dr. Nzinga Harrison 1:06:04
I had so much fun narrating the book. But yeah, so if you want to hear more of this voice, get the audible.
Casey McGuire Davidson 1:06:13
Perfect. Thank you so much.
Dr. Nzinga Harrison 1:06:14
Thank you, Casey.
Thank you for listening to this episode of The Hello Someday podcast.
If you’re interested in learning more about me, the work I do, and access free resources and guides to help you build a life you love without alcohol. Please visit hellosomedaycoaching.com. And I would be so grateful if you would take a few minutes to rate and review this podcast so that more women can find it. And join the conversation about drinking less and living more.
